The Daily Free Press recounts the HUBWeek event in which Center Director Bruce Rosen and medical illustrator Danny Quirk spoke about the intersectionality of human anatomy and visual art.
Functional Connectivity As A Possible Biomarker In Autism Spectrum Disorder
 |
|
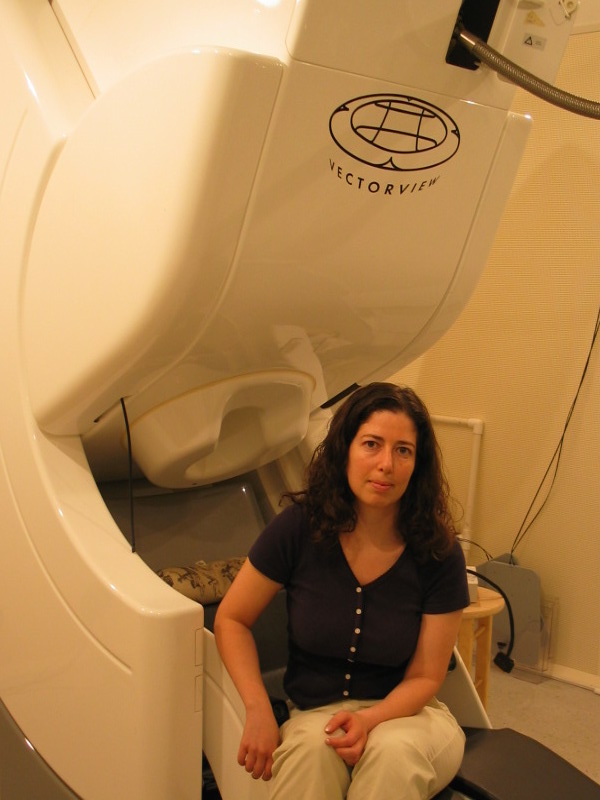
Using the imaging modality MEG, a team of researchers led by Tal Kenet – shown here with an MEG scanner – are exploring differences in the brain in autism spectrum disorder. (Image courtesy of Sheraz Khan.)
|
One in 68 children in the US has an autism spectrum disorder (ASD), according to a recent report by the Centers for Disease Control and Prevention, up from 1 in 88 only two years ago.
Better understandings of the causes of ASD would aid in diagnosis, as well as in the development of therapies and strategies to help individuals with autism. ASD has a complex genetic basis, though, and there are no clear identifying biomarkers. Currently, diagnoses are made only behaviorally, based on evaluations by developmental specialists.
Recent research has pointed to abnormalities in functional connectivity in the brain – that is, the integrated relationships between distinct regions of the brain – as a possible biomarker for ASD. But the precise nature of those abnormalities has remained elusive. Now, a team of investigators with the Athinoula A. Martinos Center for Biomedical Imaging at the Massachusetts General Hospital has found a possible approach to framing ASD based on functional connectivity. They reported their findings in a recent issue of the journal Brain.
“There is considerable disagreement about the nature of functional connectivity abnormalities in ASD, with many conflicting findings,” said Sheraz Khan, a postdoctoral research fellow in the TRANSCEND Research Group and first author of the Brain study. “We addressed this puzzle using the noninvasive imaging technique magnetoencephalography – MEG – and state of the art analyses.”
Thus far, investigators have tackled the question of functional connectivity mostly using functional magnetic resonance imaging, or fMRI. Using MEG, the TRANSCEND researchers – led by Tal Kenet, an instructor at Harvard Medical School and a principal investigator in the MGH Department of Neurology – were able to circumvent some of the confounding factors associated with the fMRI studies, including issues stemming from subject head motion in fMRI scanners.
MEG offered other advantages as well. Whereas fMRI has relatively slow temporal resolution – on the scale of half a second or so – MEG has millisecond time resolution. Such resolution was needed, Khan said, to optimally track the flow of information in the cortex in both space and time.
What the researchers found with the technique was significant. The experiments showed that long-range feedforward (bottom-up) functional connectivity was higher in individuals with ASD than in typically developing individuals, while both local and long-range feedback (top-down) functional connectivity were lower.
Importantly, they were able to blindly classify ASD participants using this approach with 90 percent accuracy, with the measures correlating with severity and other behavioral features of ASD.
Based on these findings, the investigators proposed a novel unifying framework for functional connectivity abnormalities in ASD, differentiating between top-down and bottom-up functional connectivity abnormalities.
“It is important to note that even minor changes in the feedforward/feedback ratios in ASD could significantly alter perception and cognitive processing,” Khan said. “Such altered ratios would likely be at the core of the observed sensory processing abnormalities in ASD, as well as at the core of many or most of the observed behavioral abnormalities associated with the disorder.”
The researchers are now working to validate the findings, extending the framework to other sensory modalities – beyond the tactile stimulation used in the present study – as well as to more complex processes, “to better understand whether the findings are indeed characteristic of ASD,” Khan said.
-----
Subscribe to the Martinos Center newsletter to read more about what's happening in the Center.


